In Situ PCR for the Detection of Mycobacterium avium subsp. paratuberculosis (MAP)
Introduction
In situ Polymerase Chain Reaction (in situ PCR) is a powerful technique that combines the amplification capability of PCR with the spatial resolution of histological analysis. This method enables the localization and detection of specific DNA sequences directly within tissue sections, preserving the architecture of the sample. In the context of paratuberculosis (Johne’s disease), caused by Mycobacterium avium subsp. paratuberculosis (MAP), in situ PCR allows for the detection of MAP DNA within formalin-fixed, paraffin-embedded (FFPE) tissues.
This technique has become particularly useful for identifying MAP spheroplasts, or cell-wall-deficient forms, which may escape detection through conventional staining or culture methods. As such, in situ PCR has gained interest as a highly sensitive molecular diagnostic approach that complements histopathological analysis and standard PCR.
Principle and Methodology
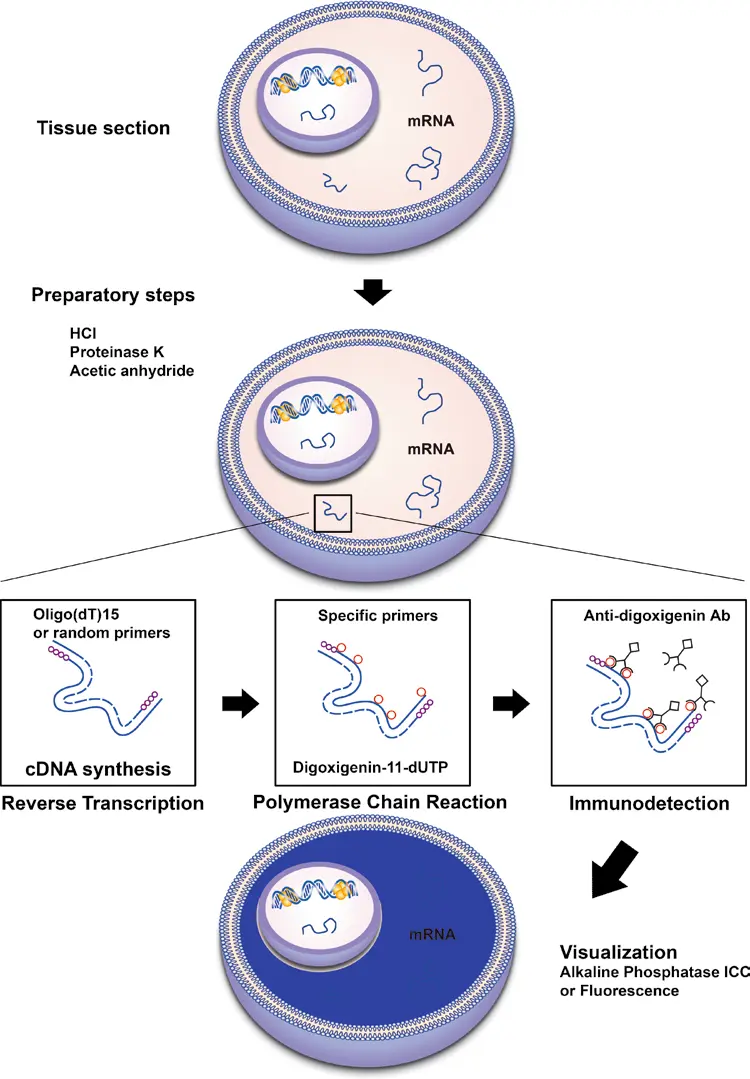
In situ PCR works by amplifying target DNA sequences within intact cells or tissues that have been embedded and sectioned for microscopy. The protocol generally includes the following steps:
- Tissue Preparation: FFPE tissue sections are mounted on microscope slides, followed by deparaffinization and rehydration.
- Permeabilization: Tissues are treated with enzymes or chemicals to increase accessibility of DNA within cells.
- DNase Treatment (optional): To reduce nonspecific amplification, some protocols include a step to remove non-genomic or fragmented DNA.
-
PCR Amplification: The slide-mounted tissues are incubated with a PCR mixture that includes:
- Sequence-specific primers targeting MAP DNA (e.g., IS900)
- DNA polymerase
- Labeled nucleotides (e.g., digoxigenin- or biotin-labeled)
-
Detection: After amplification, the newly synthesized DNA is visualized using:
- Enzymatic labeling (e.g., with alkaline phosphatase or horseradish peroxidase)
- Fluorescent in situ hybridization (FISH) for high-resolution detection under fluorescence microscopy
Unlike traditional PCR, the location of the amplified product is retained within the cell structure, allowing direct association of MAP presence with histopathological lesions.
Applications in MAP Diagnosis
1. Detection of MAP DNA in Tissue
In situ PCR enables precise localization of MAP within infected tissues, including intestine, lymph nodes, and ileocecal mucosa, even when MAP is present in low abundance.
2. Identification of Spheroplasts
MAP may exist in cell wall-deficient forms, especially in chronic infections or under antimicrobial pressure. These forms often evade detection via Ziehl–Neelsen staining or standard culture methods. In situ PCR can amplify their DNA directly from tissue, making it a valuable tool for confirming their presence (Delgado et al., 2011).
3. Confirmation of Histological Findings
It provides molecular confirmation of MAP presence in granulomatous lesions observed in tissue sections, thereby enhancing diagnostic certainty.
4. Retrospective Diagnosis
FFPE samples stored from clinical cases can be revisited with in situ PCR, allowing retrospective studies and epidemiological investigations without the need for fresh tissue.
Advantages
- High Specificity and Sensitivity: When using MAP-specific primers (e.g., targeting IS900), in situ PCR offers excellent sensitivity, even for low-copy DNA targets.
- Tissue Context Preserved: Unlike conventional PCR, in situ PCR maintains spatial integrity, allowing visualization of infection sites within the tissue.
- Versatility: Applicable to a range of tissue types, including intestinal sections, mesenteric lymph nodes, and even placental tissues in suspected vertical transmission cases.
- Detection of Non-Culturable Forms: Can detect MAP even when the bacteria cannot be cultured or visualized by staining.
Clinical and Research Implications
In situ PCR stands at the intersection of molecular biology and pathology, offering unparalleled insight into MAP pathogenesis at the cellular level. In research settings, it has been used to:
- Explore MAP's tissue tropism and invasion patterns
- Investigate early infection stages
- Study immunologically silent infections or latent MAP reservoirs
- Support diagnosis in ambiguous clinical cases where traditional tests fail
Given the growing interest in latent MAP infection in humans and its proposed link to diseases like Crohn’s disease, in situ PCR is also being explored in comparative pathology and zoonosis research
In situ PCR is a powerful diagnostic and investigative tool that provides direct, localized detection of MAP DNA within tissues, including hard-to-detect spheroplast forms. Although the method is technically demanding and not yet standardized for routine field diagnosis, its diagnostic precision and ability to reveal intracellular and non-culturable forms of MAP make it a valuable complementary technique in the diagnosis and study of paratuberculosis.
With continued refinement and automation, in situ PCR has the potential to evolve into a routine tool for confirmatory diagnostics, vaccine evaluation, and epidemiological surveillance in both veterinary and potentially human health contexts.